Global Women’s Health Innovation Program (GWHIP)
Our Faculty
Welcome Letter from Dr. Susan Harvey, Director of GWHIP
As a Global Women’s Health Innovation Program Director, I am dedicated to establishing solutions to reduce women’s suffering from cancer. Breast cancer, the most common cancer in women and the #1 cancer killer of women globally, is GWHIP first focus area. Using available technology, detection, diagnosis and treatment can occur in one visit. This innovative care model will reduce racial and regional inequities, expand to other cancer types and prove accessible, affordable and highly effective at saving women’s lives.
I take great pride in being part of the GWHIP team to revolutionize breast cancer care through our, “One woman, one clinic, one day” approach to testing and curing breast cancer.
Our Partners
Our Impact
3,000
Women’s lives saved
$8.6M
Invested in innovation for women
Past Projects
Ever since CBID was established in 2009, there has been a women’s health focused project each year.
Scroll below to read more about all our different projects!
-
THE TEAM
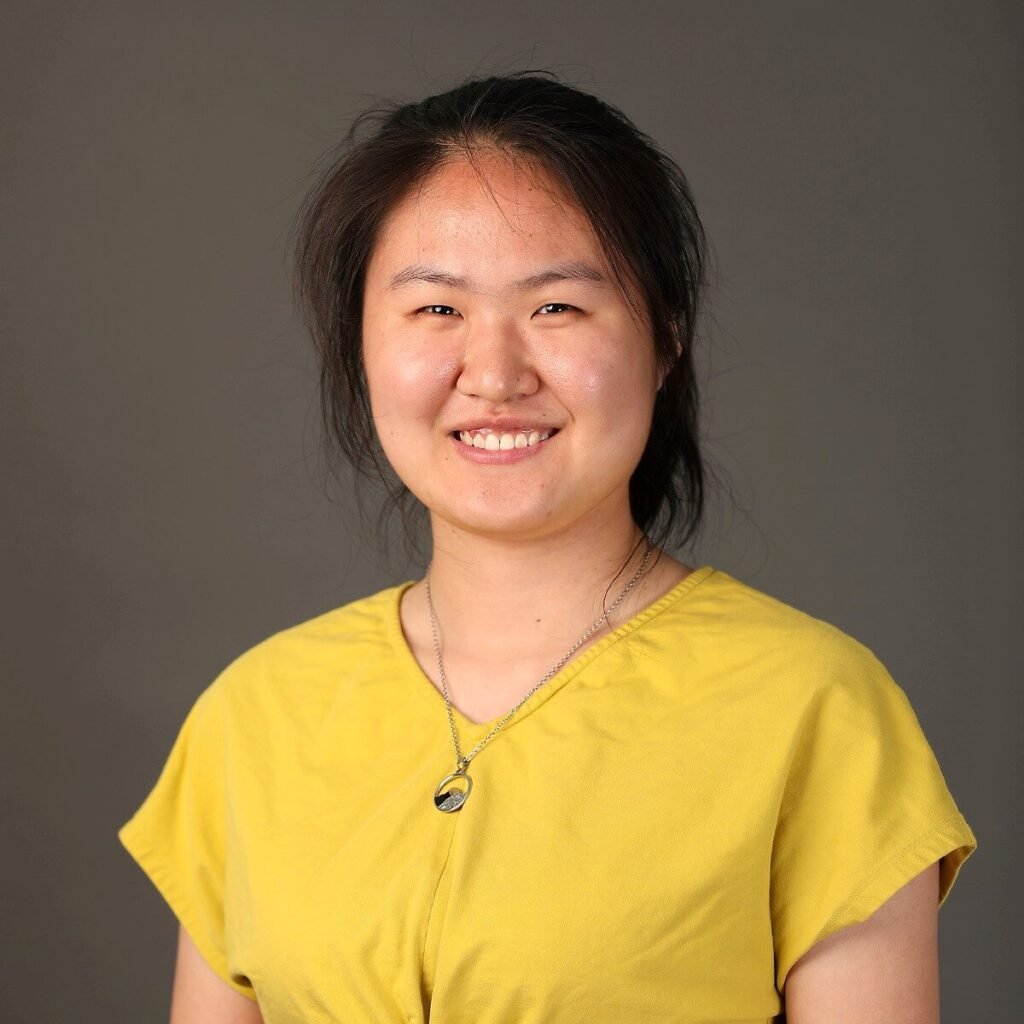
Student Team: Fujia Zheng, Shirley Lin, Sainkhuu Enkh-Otgo, Rida Amjed
Advisors: Dr. Youseph Yazdi, Dr. Soumyadipta Acharya, Dr. Susan Harvey, Samson Jarso, Dr. Sara Sukumar
ABSTRACT
Breast Cancer is the second most common and second leading cause of death for women in Sub-Saharan Africa. 6 out of 10 women die from breast cancer within 5 years of diagnosis. For women presenting a lump in their breasts, they often need to travel on average 200 km to the closest healthcare system, facing huge time and cost commitment. Even for women who make it to the healthcare centers face challenges, centers will use Fine Needle Aspiration to collect cellular samples from the lump. While cost-effective and minimally invasive, the results differ from practitioner to practitioner. An inadequate fine needle aspiration requires resampling. The inadequacy rate at rural area can go up to 80% where 77% of the population reside.
YieldEASE is an innovative biopsy accessory that can increase the accuracy of Fine Needle Aspiration in one single pass. By increasing the success rate of the first procedure, we decrease the cost for the healthcare system and the patients due to delayed diagnosis and treatment.
-
THE TEAM
Student Team: Kim Hwang, Pav Naicker, Leanne Pichay, Teja Sathi
Advisors: Youseph Yazdi, Soumyadipta Acharya, Harshad Sanghvi, Susan Harvey, Radha Taralekar, Aditya Polsani
ABSTRACT
Ekyaalo is an AI-assisted method of interpreting breast cytology from fine needle aspiration samples to increase the accessibility, speed, accuracy, and reliability of breast cancer diagnosis in low- and middle-income countries. Breast cancer is a leading cause of cancer death in women worldwide. In Uganda, breast cancer carries a 20x greater likelihood of mortality than in the United States in a 5-year period, with 1 in 2 Ugandan women diagnosed with breast cancer succumbing to the disease. Women in rural communities especially, face multiple barriers to accessing diagnosis, which contributes to precious time lost as their cancer progresses. It takes well-over the WHO guideline of 60 days for a woman to receive diagnostic results and many never do. Over 80% of women presenting for treatment in Uganda have late-stage disease which has a low survival rate even with treatment. (In contrast, in the US it is 53%). Thus, there is a need to decentralize the method of breast cancer diagnosis in order to reduce diagnostic turnaround-time and reduce mortality.
Ekyaalo intends to increase access to breast cancer diagnosis in rural resource limited communities, so that women presenting with breast cancer symptoms can receive immediate triage within traveling distance of their villages before being directed to actionable next steps in the care pathway. Stakeholder feedback that our team conducted with the 18 pathologists in Uganda established that moving preliminary diagnosis to lower-tier health centers could reduce late stage presentation of breast cancer. We aim to 1) Enable the use of fine needle aspiration cytology, which is minimally invasive, minimizes discomfort to patient, requires non-specialized resources to acquire and takes minutes to process 2) Implement digital pathology to share information between local health workers and pathologists; 3) Apply AI to enable on-site evaluation of adequacy and accurate classification of malignancy; 4) Create a standardized workflow through combination of hardware and software implementations.
-
THE TEAM
Student Team: Kim Hwang, Pav Naicker, Leanne Pichay, Teja Sathi
Advisors: Youseph Yazdi, Soumyadipta Acharya, April Zambelli-Weiner, Fred Walker, Aditya Polsani
ABSTRACT
DiscOva is a comfortable and convenient method to collect, store, and transport menstrual effluent samples, while maintaining the integrity needed for these samples to be useful for the diagnosis of gynecologic disease. Menstrual effluent’s composition of endometrial tissue, live cells, and blood makes it uniquely suited for the diagnosis of gynecologic diseases like endometriosis. More than 1 in 10 women suffer from endometriosis, which causes extreme pelvic pain and has no good method of detection. The only method of diagnosis is an invasive surgery carrying the risk of many other complications. The live cells derived from menstrual effluent have demonstrated high diagnostic potential for endometriosis. This is but one initial application, as mononuclear cells isolated from menstrual samples show a strong resemblance with biopsy-derived endometrial mononuclear cells, suggesting many other promising uses.
DiscOva seeks to take a menstruating person-centered approach keeping collection simple and removing the need for extensive sampling handling. It also preserves the components of menstrual effluent, like live cells, that are critical to diagnostics. Through strategic partnerships with researchers in the space, DiscOva embeds itself in the clinical pathway as research in this space continues to grow. Work taken to progress DiscOva has included validation of methods of preserving cell viability, specifically the stromal fibroblast cells used in endometriosis detection research. Analogs such as Streck Tubes, BD Vacutainer tubes and other similar devices in sample preservation have been studied. In parallel, DiscOva has undergone user-centered design targeted at seamless at-home collection and preservation, including extensive customer discovery and exploration into menstrual products on the market. Each of these design considerations ensures that DiscOva will address the need it seeks to fulfill adequately.
-
THE TEAM
Student Team: Ryan Bell, Brielle Cenci, Kaveri Das, Grace Weyand, Hannah Sennik, Sneha Shivkumar
Advisors: Soumyadipta Acharya, PhD; Azadeh Farzin, MD; Christopher Golden, MD; Alain Labrique, PhD; Youseph Yazdi, PhD; Aditya Polsani
ABSTRACT
Approximately 2.7 million newborns die each year. 99% of these deaths occur in low-resource settings, and 75% of these deaths occur during the first week of life. In Uganda, community health workers, or CHWs, visit the homes of newborns to assess their health during the first week of life. The CHWs check for seven danger signs that have been established by the World Health Organization (WHO). There are four qualitative signs: difficulty feeding, convulsions, chest indrawing, and movement only when stimulated; and three quantitative signs: respiratory rate > 60bpm, and temperature > 37.5°C or < 35.5°C. Identification of even one of these danger signs is indicative of severe neonatal illness, which means that the neonate should be taken to a health facility. The problem is that there are not enough CHWs to visit every newborn, which means that many neonatal illnesses go unnoticed until it is too late. Our solution is the NeMo (neonatal monitoring) system, which empowers mothers to assess their own baby’s health at home. This system aims to reduce the number of preventable neonatal deaths by improving the frequency and quality of neonatal health assessments during the first week of life. The NeMo system consists of an audiobook that guides the mother in checking for the qualitative danger signs and a wearable sensor that checks for the qualitative danger signs. The mother will use the system every day of the newborn’s first week of life, allowing for more frequent assessment of the neonate compared to the current standard of care. Watch Video
-
THE TEAM
Student Team: Alina Andrews, David Maher, Elizabeth Russo, Madeline Wartan, David Zarrin
Advisors: David Hackam, MD; May Chen, MD; Mark Kovler, MD; Emily Dunn, MD; Youseph Yazdi, PhD; Soumyadipta Acharya, PhD; Aditya Polsani, MS; Joshua de Souza, MSE; Medtronic, Minimally Invasive Therapies Group (Boulder, CO)
ABSTRACT
Necrotizing Enterocolitis (NEC) is an inflammatory disease that causes bowel necrosis in premature infants. It is the number one cause of death in infants weighing less than 1500 grams and the number one surgical emergency among all patients in the Neonatal Intensive Care Unit (NICU). 380,000 infants are born prematurely annually, with over 90,000 at elevated risk for developing NEC. This disease can onset acutely and severely, causing seemingly healthy infants to undergo surgery within 24 to 48 hours. Current diagnostic methods, which include physical examinations and abdominal X-rays, are not sensitive and specific enough to facilitate early detection of NEC. Physical examinations consist of manual abdominal girth measurements and auscultation. These assessments are both subjective and infrequent, as they occur every three to four hours. X-ray, the diagnostic gold standard, is only effective at diagnosing late-stage NEC. These limitations result in a large percentage of the 5,400 infants diagnosed with definite NEC each year to require surgical intervention since medical treatment was initiated too late. Surgical intervention carries a 30% mortality rate that results in over 800 infants dying each year. Our solution for earlier NEC detection is a novel four-quadrant abdominal patch sending output data to an algorithm that is capable of objectively and continuously monitoring the earliest physiological and clinical indicators of the disease: reduced bowel sounds and altered gut perfusion. This proprietary algorithm will continuously isolate bowel sounds from ambient and environmental noise in neonatal critical care settings to estimate gastrointestinal motility levels. A separate algorithm will analyze temporal perfusion changes by trending regional oxygen saturation (rSO2) values in real-time. In combination, these objective metrics of gut perfusion and gastrointestinal motility will guide medical management of neonates. Integrating NEC Check into the current standard of care for this patient population can quickly alert providers of changes in abdominal health.
-
THE TEAM
Student Team: Matthew Hill, Bonolo Mathekga, Mete Morris, Melissa Schweizer, Collin Shale, Digvijay Singh
Advisors: Soumyadipta Acharya, MD, MSE, PhD; Sylvia Hinrichsen, MD, PhD; Jonathan Golub, PhD, MPH; Neil Martinson, MBBCH, DCH, MFGP, MPH; Gavin Churchyard, MBBCH, FCP (SA), MMed, PhD
ABSTRACT
Each year, it is estimated that over one million children are infected with active tuberculosis (TB) resulting in over 233,000 deaths. Of these deaths, it is also estimated that 96% occur in children that were never treated for TB. Diagnostic testing used for adult tuberculosis has reduced sensitivity in children less than five years of age, and the clinical symptoms and signs of childhood TB overlap with many other childhood diseases. In Sub-Saharan Africa, this problem is further complicated by the current HIV epidemic as children with both HIV and TB are at risk of developing extrapulmonary TB. Childhood TB is specifically difficult to differentiate from other lower respiratory tract infections (LRTIs) in children with recent evidence indicating that childhood TB is especially missed in children presenting with symptoms of acute pneumonia.
TB-D is researching and developing a solution to assist healthcare providers in correctly differentiating childhood TB from other LRTIs. In the SubSaharan Africa context specifically, healthcare providers rely on patient history and clinical investigations in order to determine how likely a child is to have TB. Depending on the level of suspicion, healthcare providers will order diagnostic testing for children or even begin empirical treatment; however, when healthcare providers suspect a different LRTI, they may begin treatment for the wrong LRTI. This improper diagnosis leads to diagnostic delay for children with TB along with lost follow-up among children that seek alternate care sources. TB-D is developing a solution that will assist healthcare providers in correctly suspecting TB within children, resulting in increased detection and treatment of childhood TB.
Our team has conducted observations across multiple levels of care in South Africa in order to validate the need and assess current provider practices for investigating children with LRTIs. Healthcare providers across primary, outpatient, and inpatient care have confirmed the current difficulties with differentiating childhood TB from other LRTIs. Moving forward, the team will be focused on testing prototypes with users and validating the efficacy of our design in precisely identifying children with TB.
-
THE TEAM
Student Team: Anthony Ho, Shababa Matin, Natalie Ng, Madison Vanosdoll, Allison Wallingford, Ryan Xu
Advisors: Soumyadipta Acharya, MSE, MD, PhD; Christopher Golden, MD; Alain Labrique, PhD; Peter Waiswa, MPH, PhD; Moses Kyangwa; Azadeh Farzin, MD
ABSTRACT
Each year, 3.3 million newborns die in the first 28 days following birth, with 75% of these deaths occurring in the first seven days of life. A majority of these deaths occur within homes in low-resource settings, largely due to preventable causes such as pneumonia, sepsis, and other illnesses. Healthcare systems in low-resource settings often rely on volunteer community health workers (CHWs) to visit newborns in rural villages in the first week of life for triage. CHWs triage newborns based on the World Health Organization’s established Integrated Management of Newborn and Childhood Illness (IMNCI) danger signs: difficulty breastfeeding, convulsions, chest indrawing, movement only when stimulated, respiratory rate greater than 60 breaths per minute, temperature higher than 37.5 ˚C, and temperature less than 35.5 ˚C. The number of CHWs, however, remains woefully inadequate and thus infants with signs of illness are often identified too late to impact survival. Although effective identification of these signs at the community level can intercept illness and incite care-seeking behavior capable of impacting child mortality, the tools and training needed to assess quantitative and qualitative indicators of illness are lacking in low-income settings.
Therefore, our team has developed the NeMo system, a two-part neonatal monitoring system designed to empower mothers, regardless of literacy, to effectively identify danger signs in their newborns and guide them to take appropriate and timely action to seek care outside the home. This system is comprised of a low-cost wearable band that measures the newborn’s respiratory rate and temperature and is paired with a smartphone application that guides the mother through the qualitative danger signs. Our team has travelled to Uganda to validate the usability of this system and tailor-fitted the NeMo system to the end user. Currently, the NeMo system is undergoing validation testing in the Johns Hopkins Nursery where data collection enables breath-by-breath analysis to iteratively improve the respiratory rate algorithm’s overall sensitivity and specificity. The team will return to Uganda to perform an acceptability study where mothers will be observed under the intended use case to study barriers of adoptions and behavior change triggered by the NeMo system.
-
THE TEAM
Student Team: Rachel An, Andrew Jann, Matthew Lerner, Polly Ma, Mohit Singhala
Advisors: Soumyadipta Acharya, MD, PhD; Azadeh Farzin, MD; Christopher Golden, MD; Alain Labrique, PhD; Youseph Yazdi, PhDABSTRACT
Approximately 2.7 million newborns die each year, with 75% of these deaths occurring during the first week of life. One approach to tackle this problem has been to send community health workers, or CHWs, to the home to assess the neonate during this high risk period. The CHW assesses the neonate based on the WHO guidelines: difficulty feeding, convulsions, chest indrawing, movement only when stimulated, respiratory rate greater than 60bpm, and temperature greater than 37.5°C or less than 35.5°C. Identification of even one of these danger signs is indicative of severe neonatal illness and result in referral of the neonate to a facility. However, the limited number of community health workers and infrequency of visits create a bottleneck, and the timing of proper assessment aligning with the onset of symptoms is happenstance. During the times in the first week when the CHW is not present, sick neonates may be identified too late to impact survival. By improving the frequency and quality of neonate assessment during the first week of life, our innovation aims to tackle preventable neonatal deaths caused by delayed identification of illness. NeMo (neonatal monitoring) aims to task-shift neonatal assessment from CHWs to mothers and provide tools for them to identify neonatal illness in the first week of life. The NeMo system consists of a smartphone application to guide the mother through the assessment based on the evidence-based WHO guidelines and a proprietary ultra low-cost disposable sensor that measures the respiratory rate and temperature of the neonate. The mother will use the system everyday for the first week of the neonate’s life, allowing for more frequent assessment of the neonate compared to the current standard of care.
-
The Team
Student Team: Chanya Elakkad, Joseph Pia, Victor Yu and Sam Zschack
Clinical Advisors: Soumyadipta Acharya, Youseph Yazdi, Alain Labrique, Azadeh FarzinAbstract
Over 66% of newborn deaths happen during the first week of life due to the fragile immune system of the neonates that results in the rapid development of fatal conditions. In lower income countries, the majority of the population receives their primary health care by trained community health care workers (CHWs). The majority of births in the developing world occur at home, so the CHWs are critical to providing clinical assessments and referrals to healthcare facilities. Despite proven success of this intervention, the limited number of trained CHWs and frequency of visits creates a bottleneck for care. Because of this, the timing of proper assessment aligning with the onset of symptoms is happenstance. One caregiver that is not limited in their ability to monitor the neonate is the mother. We identified theunmet need to design interventions to improve maternal recognition of neonatal illness at home and prompt care seeking behavior.
A task shifting of neonatal assessment and recognition of danger signs to mothers is a promising strategy to improve early identification of neonatal illness. To accomplish this our team has developed INFORM (INfant monitoring FOR Mothers), a system that provides reliable and consistent monitoring of infants for identification of danger signs of severe illness during the critical first week of life to facilitate early referral of sick neonates. INFORM consists of two parts – an Interactive Voice Response (IVR) based mHealth platform and a low cost reusable wearable device. CHWs can enroll mothers into this system and provide them with the wearable device close. Once the mother or a family member notifies the system that she has given birth through a simple SMS or call, INFORM’s mHealth platform places a voice call to the mother or family of a newborn infant every day during the critical first seven days of life, starting a “virtual CHW visit”. The system will walk a mother through a clinical assessment of her baby and the wearable device will provide accurate measurements of the critical vital signs, temperature and breathing rate. Using this system, mothers will finally be empowered to identify severe neonatal illness effectively and in a timely manner.
-
The Team
Student Team: Kendall Covington, Sakina Girnary, Teja Maruvada, Ramji Rengarajan, Kavya Singampalli
Clinical Advisors: Soumyadipta Acharya, MD, PhD; Rashmi Asif, MBBS; Cherrie Evans, CNM; Tor Inge Garvik, MS; Jennifer Gilbertson, MSE; Lindsay Litwin, MPH; Pushkar Ingale, MDes; Swati Mahajan, MBBS, MPH; Harshad Sanghvi, MD; Pallavi Sinha, MBBS; Rachel Willardson, MSAbstract
Each year, 350,000 women and 2 million babies die from birth-related complications. In India specifically, the UN Millennium Development Goals 4 and 5 aim to reduce high infant mortality rates, decrease the maternal mortality ratio, and increase birth attendance by skilled health professionals. To achieve this, nursing schools that are currently training students using a standardized curriculum have recently added Skills Labs to expose students to skill-based and simulation-based training practice, apart from a clinical internship during the final year of nursing education. However, many of the labour monitoring skills taught in the curriculum are not translated to the clinical site due to the lack of interactive, immersive and integrated training. This leads to a lack of nurse empowerment to make important decisions in emergent situations that can save both the mother and child.
We have developed a training system to improve the current labour monitoring training system by integrating the measurement, recording, interpreting and acting aspects, habituating nursing students to make more timely measurements and decisions, and encouraging a low-dose high-frequency training approach without the need for direct faculty involvement. Our device, Physim, allows students to practice and learn measurements, plot data onto a partograph, and make decisions throughout the progress of labour. It incorporates a physical model containing modules for fetal heart rate, contractions, and cervical dilatation, which connects to a flipbook user interface where the user plots data on a partograph. After each measurement is complete, the student assesses the parameters to ensure that labour is progressing normally and appropriate actions are taken.
PhySim offers significant advantages over the traditional case study approaches by encouraging dialogue and discussion among the students and enhancing the learning for both the user and the operator. PhySim also incorporates group-based simulation, that has been shown extensively to improve learning comprehension and retention.This system habituates the student to take measurements in a timely manner, make decisions at each time point after measurements are taken, and contextualize those measurements in the progression of labour. By providing exposure to both the normal and abnormal progression of labour in the training setting using a low dose high frequency training routine, students will be able to build their confidence before reaching the clinical site, and will be better-equipped to make evidence-based decisions in practice.
-
The Team
Student Team: Wes Bernier, Allie Sibole, Melody Tan, and Jackie Wanjala
Clinical Advisors: Azadeh Farzin, MD, Kusum Thapa, MD, Neena Khadka, MD, Lindsay Litwin, and Kristy PetersonAbstract
In overcrowded neonatal care units where each caregiver is responsible for many babies, there is a serious risk of neonatal distress going unnoticed. Traditional newborn vital sign monitors can alert providers to subtle indications of illness but are too expensive for hospitals in low-resource settings and ineffective in understaffed facilities. We observed this problem firsthand in Nepal and Indonesia and identified a need for caregivers in neonatal units to be able to tell when babies are experiencing vital sign abnormalities in order to know when they are in need of immediate intervention.
As a team of master’s students at the Johns Hopkins Center for Bioengineering Innovation & Design, we are in the process of developing a newborn vital signs monitor for low-resource settings. Our system has three components:
- Wearable vital signs sensors to measure heart and respiratory rate, with potential to add temperature and oxygen saturation monitoring in the future. These sensors are designed to have minimal contact with the baby in order to protect their fragile skin.
- A centralized interface tablet that receives wireless signal from the sensors and displays the vital signs of all the babies in the unit. The centralized interface design would be more affordable than individual patient monitors.
- A paging system to alert caregivers when a baby is in need of immediate attention. From our field observations, we observed that nurses are not always present in the unit. This alert system will enable providers to know if a baby is experiencing distress even if they are not within audible range of the alarm.
We believe that this system will enable earlier detection of neonatal distress, leading to earlier, more effective interventions and alleviating the burden on overworked caregivers.
-
The Team
Student Team: Kimber Ashman, Aaron Chang, Ian Graham, Nichaluk Leartprapun, Patience Osei, Mihika Reddy
Clinical Advisors: Barrett Yates, MSE, Sunny Chen, Tor Inge Garvik, MSc, Cherrie Evans, CNM, MSN, DrPH, Kusum Thapa, MD, FRCOG, MPH, Blami Dao, MD, Annie Clark, CNM, MPH, Harshad Sanghvi, MDAbstract
Many caesarean sections are preventable. During our August field immersion trips in Nepal and India, we witnessed high rates of caesarean sections and low rates of instrumental deliveries. In low- and middle-income countries, caesarean sections not only increase costs, but also maternal and fetal morbidities. From the discussions we have had with OBGYNs and midwives in India and Nepal, along with members in the public health sector, we have recognized that a key contributor to the high prevalence of caesarean sections is the lack of training in managing the progression of the second stage of labor and performing assisted deliveries. Many midwives and skilled birth attendants do not have the confidence to perform proper fetal head assessments during vaginal exams, which is critical to the decision-making process for appropriate referral for assisted delivery. Currently, there are no low-cost labor management training simulators for LMICs that adequately teach fetal head assessment.
Our team is creating a low-cost simulation tool that provides a method of safely practicing the vaginal examination skills that are essential to clinical decision making during the second stage of labor. Our device will help teach proper assessment of fetal head position, station, orientation, and moulding during a vaginal exam. We hope to enable midwives and SBAs to feel more confident in managing labor by allowing them to practice the skills that are vital to appropriate decision making and thereby prevent unnecessary caesarean sections.
-
The Team
Student Team: Eric Ashuckian, Jennifer Gilbertson, Julia Michalow, Matthew Petney
Clinical Advisors: Azadeh Farzin, MD, Department of Neonatology; Wilson Wang, MD, Jhpiego Indonesia; Elizabeth Cristofalo, MD, Department of Neonatology
Advisors: Kristy Peterson, Product Develop Manager, Jhpiego; Lindsay Litwin, Senior Program Coordinator, Jhpiego; Luke Mullany, PhD, Department of International Health, Bloomberg School of Public Health; Joanne Katz, ScD, MS, Department of International Health, Bloomberg School of Public Health; Pushkar Ingale, Laerdal Global Health, India; Jinjie Sunny Chen, Laerdal Global Health, Norway; Tor Inge Garvik, Laerdal Global Health, Norway
Abstract
Neonatal hypothermia affects an estimated 17 million newborns annually in developing countries. It is a significant contributing factor to the high rates of neonatal mortality that exists in this setting because hypothermia compromises neonates’ immune systems, thus increasing their susceptibility to other conditions such as infection and hypoglycemia. In Nepal neonatal hypothermia is the fourth leading cause of neonatal death and 16 percent of hypothermic neonates die during the first week after birth.
Despite high incidence rates for hypothermia, caretakers are frequently unaware of its occurrence because the early stages of hypothermia are asymptomatic. Our team has developed the IllumiNate hat to monitor neonatal temperature and alert care providers when newborns become hypothermic. The hat uses a low cost circuit that lasts for a minimum of three days, the highest risk period for hypothermia and its associated mortality. The alert is designed to be easily interpreted by non-literate mothers. Field studies in Nepal, Tanzania, and India have confirmed the need for hypothermia prevention and monitoring, and have guided the team’s design process. Bench-top testing has additionally demonstrated that the technology is comparable to the standard of care. The IllumiNate hat will be implemented with a training program on hypothermia prevention and management, and will empower mothers to monitor their babies for hypothermia, one of the most risky and easily corrected conditions that newborns face.
-
The Team
Student Team: Melissa Diskin, Jan Lee, Pankti Shah, Barrett Yates
Clinical Advisor: Cherrie Evans, DrPH, CNM, Jhpiego
Advisors: Helge Fossan, Laerdal Global Health, Norway; Jinjie Sunny Chen, Laerdal Global Health; Harshad Sanghvi, MD, Jhpiego; Lynn Kanyuuru, MD, Jhpiego; Kristy Peterson, Jhpiego
Abstract
Each year, two million babies die annually from intrapartum-related deaths. Another one million are born with defects caused by birth asphyxia. To prevent complications the World Health Organization recommends that providers measure and record fetal heart rate every 30 minutes. The fetal heart rate provides critical information that determines if an intervention needs to be performed. Studies have shown that up to 43 percent of intrapartum neonatal deaths could be related to inadequate fetal heart rate monitoring. The current monitoring device, the Pinard horn, is inaccurate, time-consuming, fatiguing and difficult to use. When providers are unable to effectively monitor fetal heart rate during labor, it compromises the providers’ abilities to take action.
In partnership with Jhpiego and Laerdal Global Health, the design team has developed the Sikia monitor, an electronic fetal heart rate monitor that plays the fetal heart sound and displays heart rate. By using simple, inexpensive microphone technology, providers will have a faster, easier, and more accurate way to measure fetal heart rate. The team has recorded fetal heart sounds, improved signal quality, and has started developing an algorithm to calculate heart rate. The team has also received feedback by conducting interviews with midwives through Jhpiego, and through field visits to hospitals in India, Nepal, and Kenya. Additionally, the team has designed a study at a high-volume facility in Thika, Kenya to be performed this May. This study will provide additional users validation and feedback and quantify the value of the Sikia monitor over other devices. Overall, the Sikia monitor will increase the frequency of fetal heart rate measurement during labor, allowing for more timely interventions and thereby reducing the incidence of stillbirths and neonatal morbidity.
-
The Team
Student team: Joshua Budman, Kevin Colbert, Aaron Enten, Michael Parlato, Ashley Polhemus
Advisors: Harshad Sanghvi, MD, Jhpiego; Soumyadipta Acharya, MD, PhD
Abstract
Anemia in Developing Countries
Anemia during pregnancy is defined as hemoglobin (Hb) concentration less than 10g/dL. Maternal anemia affects more than half of the pregnant women worldwide, causing 100,000 maternal deaths and 600,000 neonatal deaths each year. It also leads to poor outcomes for the child in the form of preterm birth, low birth weight, malnutrition, and stunted cognitive development. If it is identified early, cost effective therapies can combat the effects of anemia on the mother and the child. In fact, ferrous sulfate tablets have been shown to cure anemia if the patient is adherent. However, low adherence (<50 percent in many Asian and African countries) has been reported among pregnant women. In these populations, anemia is rarely caught early in pregnancy. If women are screened regularly, they can be informed of their anemic status and may be more likely to adhere to their recommended iron supplementation regimen. HemoGlobe: A Point of Care Hemoglobin Assessment Tool
HemoGlobe is a new paradigm in preventative medicine that will empower community health workers to take anemia screening to the doorstep of rural women. A low-cost, noninvasive sensor passes multiple monochromatic lights through the finger and onto a photo detector. Using principles of photoplethysmography, the device collects the transmitted light and processes the resulting waveform. The device then connects to a cell phone, allowing real time analysis of the waveform and classification of the patient as having severe, moderate, or mild anemia. Preliminary results are based on waveforms that were collected from approximately 500 patients in Nepal and eastern India. These waveforms were subjected to a variety of nonlinear regression techniques, neural networks, and a support vector machine to develop the calibration curve.After the waveform is collected patient data can be documented on the cell phone and, along with their anemia assessment, sent to a central server via SMS, MMS, phone call, or email. Uploading this data either to a server or the cloud creates a real-time database of anemia prevalence and distribution. This database can be used to track progress in areas with a disproportionate burden of maternal anemia, as well as facilitate resource allocation decisions by public health organizations. Use of this device on an international scale has the potential to reduce rates of maternal mortality, prevent premature births, and increase the health of young children in developing countries by facilitating point of care medical assessment and education for mothers with limited access to healthcare.
-
The Team
Student Team: Stephen Dria, Kaitlyn Harfmann, Christopher Lee, David Narrow
Clinical Advisors: Janine Bullard, MD, Department of Neonatology, JHU
Other Advisors: Helge Myklebust, Harshad Sanghvi, MD
Sponsors: Day of Birth Alliance (CBID, Jhpiego & Laerdal Global Health)
Abstract
Annually, there are over 4 million global neonatal deaths primarily occurring in resource-constrained environments. This accounts for over 38% of deaths in children under the age of five. When performed properly, neonatal resuscitation is an effective means to revive newborns that are unable to properly breathe. Statistics indicate that birth asphyxia accounts for 23% of all neonatal deaths. Additionally, another one million newborns suffer from permanent disabilities due to insufficient oxygen at time of birth. Effective newborn resuscitation alone can prevent millions of newborn deaths. Neonatal resuscitation requires the use of a ‘bag-valve-mask’ or BVM. The BVM channels ambient air from the atmosphere into a one-way valve, when the user compresses the bag-component. Gas is then expelled through the mask and into the trachea, bronchus and lungs of the infant. Due to the technical difficulties associated with the procedure, newborns that otherwise would have been resuscitated die because of ineffective equipment operation and improper technique—a function of the burden of training and skill retention. Thus, it is critical to reduce the amount of skill required for providing an effective and consistent resuscitation, especially in peripheral health care centers of the developing world.
Failed resuscitations are attributed to poor head positioning and an inadequate seal between the mask and the baby’s mouth. However, air is forcibly pushed into the lungs through ventilation only ;when proper mask seal and head positioning are addressed together. After significant research, chest rise is a variable that is most cost-effective to quantify successful resuscitation instantaneously. Thus, a tool to quantify lung expansion would be revolutionary to the resuscitation protocol, providing low-skilled health workers real-time feedback throughout the procedure. Our innovation will mitigate existing inadequacies attributed to constrained resources, diminished skill retention over time and difficulty using devices associated with resuscitation. Our technical solution quantifies chest expansion and guides the user through a proper resuscitation, improving the results of attempted resuscitations and successfully managing birth asphyxia.
-
The Team
Student Team: Anjana Sinha, Hector Neira, Qing Xiang Yee, Vaishakhi Mayya
Clinical Advisors: James Shin and Ashley Cimino-Mathews, MD. Dept of Pathology Melissa Suzzane Camp, MD MPH, Johns Hopkins Breast Center
Abstract
Patients undergoing Breast Conserving Surgery (BCS) have a one in five chance of requiring a reoperation because surgeons cannot determine if the entire tumor has been removed. Surgeons rely on pathologists to assess margins through histological evaluation. Due to the inherent mechanical properties of breast tissue, this cannot be done before the surgery ends. ClearView allows pathologists to produce high-quality histology slides within minutes, enabling intra-operative assessment of tumor margins. This could prevent up to 66,000 unnecessary BCS procedures in the U.S. annually.
Using ClearView, a typical surgery will require $120 of disposables, covered by insurance companies under existing reimbursement codes. According to FDA regulations, ClearView is a Class I device, the lowest-risk device category. This affords a quick time to market, with minimal testing and regulatory requirements. Our team is collaborating closely with leading clinicians from the Johns Hopkins Breast Center, who are excited about our initial results.
-
The Team
Student Team: Anastasia Borok, Adam Clark, Luke Jungles, Nathaniel Moller
Clinical Advisors: Harshad Sanghvi, MD and Kusum Thapa, MD
Sponsor: Jhpiego and Laerdal Global Health
Abstract
Postpartum hemorrhage (PPH) is the leading cause of maternal mortality worldwide. There are over 14 million cases of PPH every year, and approximately 125,000 of these end in death. The majority of these deaths occur in resource-constrained settings, with half occurring in sub-Saharan Africa and one third in South Asia. Additionally, there are over 20 million women living with chronic illnesses (such as anemia) resulting from PPH. Tragically, a child is 10 times more likely to die before their second birthday if their mother dies from PPH. PPH is largely manageable with access to adequate resources, but these are often unavailable in remote locations. We have developed two separate solutions that will buy time for a woman to get to a care facility to receive appropriate treatment.
The Automatically-Deflating Air Postpartum Tamponade (ADAPT) is the first air-inflated tamponade and is equipped with a custom designed balloon which is inserted into the uterus and inflated to provide uniform pressure along the uterine wall. Additionally, the ADAPT automatically releases pressure, which allows the uterus to contract to its normal state while maintaining pressure against the uterine walls. The ADAPT incorporates the safety and performance of devices used in the developed world, at a cost of less than $10.
Legloves are one-size-fits-all elastic devices that are placed over the toes of a woman and rolled up the leg to her upper thigh. The compressive force along the length of the leg shunts blood away from the extremities to critical organs in the same way an anti-shock garment does. Studies have shown that shunting blood from the lower extremities to critical organs provides the equivalent of a self-transfusion of one pint of blood.
-
The Team
Student Team: Creighton Petty, Brian Rayburn, Geoffrey Russell, Lauren Smith
Clinical Advisors: Jean Anderson, MD, and Jeff Smith, MD, Department of Gynecology and Obstetrics; Cherrie Evans, [D.PH](http://d.ph/), CNM, Jhpiego
Sponsor: Jhpiego and Laerdal Global Health
Abstract
Every year, there are approximately 2 million stillbirths and neonatal deaths related to intrapartum causes. Nearly 99% of these mortalities occur in developing countries. One contributor to this disparity in global neonatal death rates is a lack of monitoring the fetal status during labor in developing countries. Though fetal heart rate is a widely accepted indicator of fetal wellbeing, it is rarely accomplished in low-resource facilities due to the lack of efficient equipment for monitoring, the low staff-to-patient ratios, the minimal staff training, and the insufficient time for finding and counting fetal heart beats. Our BabyBeats fetal monitor is a hand-held device that processes heart sounds using low-cost microphone technology and outputs heart rate on a digital display. It includes a speaker to play heart sounds that are frequency-shifted to make them easier to hear. It also uses a rechargeable cell phone battery to avoid power dependence and has durable housing to withstand harsh environments. Preliminary testing shows promise the device will enable health workers to find the fetal heart rate more quickly and reliably, without specialized training, and at a cost that enables widespread distribution.
-
The Team
Student Team: Marton Varady, Shuja Dawood, John Sidhom
Sponsor: Jhpiego
Abstract
Cervical cancer is the third most common cancer in the world where 88% of all cases occur in the developing world. With approximately 600,000 new cases every year, this silent killer is responsible for over 250,000 deaths per year, making it the second leading cause of female cancer deaths in developing countries. While cervical cancer has largely been eradicated in the developed world with the incorporation of regular screening and new opportunities for vaccinations, it remains a large burden in the developing world due to inadequate healthcare infrastructure, high costs, and the lack of an appropriate technology for treatment. Momo Scientific is a social venture medical device company dedicated to the prevention of cervical cancer. The CryoPop is a patent-pending low-cost medical device which uses dry ice for the treatment of cervical pre-cancerous lesions in low-resource settings. The CryoPop relies only on carbon dioxide tanks, readily available in developing countries because of soda companies, and is ten times cheaper, 30 times more efficient, and more effective and reliable than current technology.