2012
Global Health Innovations
-
The Team
Student Team: Anastasia Borok, Adam Clark, Luke Jungles, Nathaniel Moller
Clinical Advisors: Harshad Sanghvi, MD and Kusum Thapa, MD
Sponsor: Jhpiego and Laerdal Global Health
Abstract
Postpartum hemorrhage (PPH) is the leading cause of maternal mortality worldwide. There are over 14 million cases of PPH every year, and approximately 125,000 of these end in death. The majority of these deaths occur in resource-constrained settings, with half occurring in sub-Saharan Africa and one third in South Asia. Additionally, there are over 20 million women living with chronic illnesses (such as anemia) resulting from PPH. Tragically, a child is 10 times more likely to die before their second birthday if their mother dies from PPH. PPH is largely manageable with access to adequate resources, but these are often unavailable in remote locations. We have developed two separate solutions that will buy time for a woman to get to a care facility to receive appropriate treatment.
The Automatically-Deflating Air Postpartum Tamponade (ADAPT) is the first air-inflated tamponade and is equipped with a custom designed balloon which is inserted into the uterus and inflated to provide uniform pressure along the uterine wall. Additionally, the ADAPT automatically releases pressure, which allows the uterus to contract to its normal state while maintaining pressure against the uterine walls. The ADAPT incorporates the safety and performance of devices used in the developed world, at a cost of less than $10.
Legloves are one-size-fits-all elastic devices that are placed over the toes of a woman and rolled up the leg to her upper thigh. The compressive force along the length of the leg shunts blood away from the extremities to critical organs in the same way an anti-shock garment does. Studies have shown that shunting blood from the lower extremities to critical organs provides the equivalent of a self-transfusion of one pint of blood.
-
The Team
Student Team: Creighton Petty, Brian Rayburn, Geoffrey Russell, Lauren Smith
Clinical Advisors: Jean Anderson, MD, and Jeff Smith, MD, Department of Gynecology and Obstetrics; Cherrie Evans, [D.PH](http://d.ph/), CNM, Jhpiego
Sponsor: Jhpiego and Laerdal Global Health
Abstract
Every year, there are approximately 2 million stillbirths and neonatal deaths related to intrapartum causes. Nearly 99% of these mortalities occur in developing countries. One contributor to this disparity in global neonatal death rates is a lack of monitoring the fetal status during labor in developing countries. Though fetal heart rate is a widely accepted indicator of fetal wellbeing, it is rarely accomplished in low-resource facilities due to the lack of efficient equipment for monitoring, the low staff-to-patient ratios, the minimal staff training, and the insufficient time for finding and counting fetal heart beats. Our BabyBeats fetal monitor is a hand-held device that processes heart sounds using low-cost microphone technology and outputs heart rate on a digital display. It includes a speaker to play heart sounds that are frequency-shifted to make them easier to hear. It also uses a rechargeable cell phone battery to avoid power dependence and has durable housing to withstand harsh environments. Preliminary testing shows promise the device will enable health workers to find the fetal heart rate more quickly and reliably, without specialized training, and at a cost that enables widespread distribution.
-
The Team
Student Team: Marton Varady, Shuja Dawood, John Sidhom
Sponsor: Jhpiego
Abstract
Cervical cancer is the third most common cancer in the world where 88% of all cases occur in the developing world. With approximately 600,000 new cases every year, this silent killer is responsible for over 250,000 deaths per year, making it the second leading cause of female cancer deaths in developing countries. While cervical cancer has largely been eradicated in the developed world with the incorporation of regular screening and new opportunities for vaccinations, it remains a large burden in the developing world due to inadequate healthcare infrastructure, high costs, and the lack of an appropriate technology for treatment. Momo Scientific is a social venture medical device company dedicated to the prevention of cervical cancer. The CryoPop is a patent-pending low-cost medical device which uses dry ice for the treatment of cervical pre-cancerous lesions in low-resource settings. The CryoPop relies only on carbon dioxide tanks, readily available in developing countries because of soda companies, and is ten times cheaper, 30 times more efficient, and more effective and reliable than current technology.
-
The Team
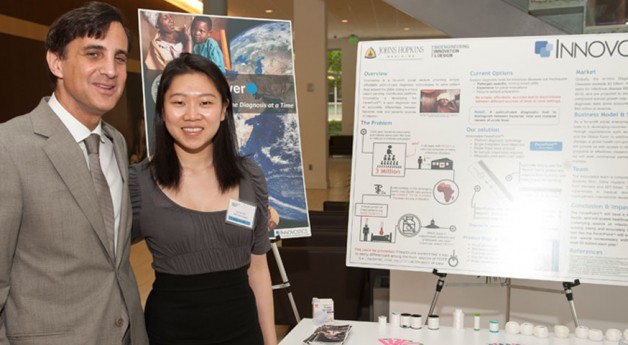
Student Team: Divya Maxwell, Luccie Wo, Luis Soenksen, James Barger, Omid Akhavan
Clinical Advisors: Stefan Riedel, MD PhD and Robert Hamilton, PhD, Department of Pathology, JHU
Sponsor: JhpiegoAbstract
Globally, malaria and bacterial pneumonia claim the lives of 3 million children under the age of five. Patients suffering from these diseases present with several symptoms, fever being the most common. Other causes of fever include influenza, dengue, and typhoid. However, healthcare providers often lack diagnostic tools to determine the underlying cause of fever, leading to misdiagnosis and over-prescription of antibiotics and other drugs. Unfortunately, 90% of these unnecessary antibiotic prescriptions occur in the developing world. Our team is developing the FeverPoint™, a lateral-flow immunoassay test to differentiate between bacterial, viral and malarial infection. Using an ultra-low-cost microfluidics platform, our test can provide results with a single drop of blood, requiring no electricity, water, or sample preparation. Our goal is to provide accurate diagnosis and to save millions of lives around the globe.
U.S. Healthcare Innovations
-
The Team
Student Team: James Barger, Divya Maxwell, Brian Rayburn, and Luccie Wo
Clinical Advisors: Clifford Weiss, MD, CBID Clinical Director; Mark Lessne, MD, Department of Radiology, JHU; Robert Liddell, MD, Interventional Radiology, Mercy Hospital, Baltimore
Abstract
Over 2 million stents are placed annually to preserve blood flow in a vessel or shunt blood to an alternative path. Current stents fail because they are static and unresponsive to physiological changes in the body, compromising the outcome of stent therapy. NeoPersona has created the novel NeoStent that adapts to the body’s demands. Similar to a pacemaker, a physician can “fine-tune” the flow within the stent during clinic visits, adapting the stent to best suit the patient’s needs. This is a platform technology that can be applied to an assortment of stents placed today, including TIPS (Transjugular Intrahepatic Portosystemic Shunt) stents, biliary stents, pediatric stents, pulmonary stents, peripheral venous stents, and cardiac stents.
The NeoStent, consists of two components: (1) Implantable — the implantable portion of the Neostent includes any commercially available stent and a nylon band which can constrict and expand the stent with the use of a piezoelectric motor; (2) External Control Box — the external control of the piezoelectric motor will be achieved with the generation of a high frequency electric field. A very specific frequency will be generated to resonate with the motor.
-
The Team
Student Team: Anastasia Borok, Creighton Petty, Lauren Smith, Marton Varady
Clinical Advisor: Andrew Lane, MD, Department of Otolaryngology, JHU
Abstract
Approximately 10 million Americans suffer from chronic sinusitis, the persistent inflammation of the sinus lining. The disease results in facial pressure, fatigue, and headaches that severely impair quality of life. Patients attempt to manage sinus inflammation with steroid sprays and irrigations, but current solutions are inadequate because they fail to reach the diseased areas. Each year, approximately 500,000 patients resort to surgery, and up to one third experience recurrent symptoms post-surgery. The SinuGlide is a novel drug delivery device that will improve post-surgical outcomes and could ultimately prevent the majority of chronic sinusitis surgeries. The SinuGlide overcomes the inadequacies of existing treatments by ensuring that medication is distributed to the affected sinus surfaces daily. The device consists of a small, specialized catheter that is inserted in the nasal cavity by the physician. The patient uses a separate external device for daily medication delivery via the catheter. A novel magnetic interface between the inserted tube and external device allows the inserted device to be placed far into the nasal passage where it cannot be seen or felt. Initial testing to date has largely mitigated the technical risks of the device and shown promise that the SinuGlide will achieve drug coverage to the majority of diseased sinus tissue.
-
The Team
Student Team: Adam Clark, Shuja Dawood, Luis Soenksen, Nathaniel Moller
Clinical Advisors: Clifford Weiss, MD, and Steven Hsu, MD, Department of Radiology, JHU
Abstract
Every year, more than 90,000 patients die unnecessary deaths due to complications of a life-sustaining medical device called a central venous catheter (CVC). Bacteria are prone to growing on CVC surfaces, causing blockages and infections, which cost hospitals $56K per case, and US healthcare $2.3 billion every year. Current solutions are expensive and only address infections or blockages, never both. With leading physicians at Johns Hopkins Hospital, Salveo Vascular has invented the Sonicade, a medical device that attaches to any CVC and prevents bacterial formation using high-frequency vibrations. Our platform technology is the first to reduce both infections and blockages in the growing $780 million dollar CVC market. The Sonicade will reach the market in 3 years and begin saving the lives of healthcare’s most vulnerable patients.
-
The Team
Student Team: Omid Akhavan, Luke Jungles, Geoffrey Russell, John-William Sidhom
Clinical Advisor: Daniel Valaik, MD, Department of Orthopaedics, JHU
Abstract
Artificial knee joints suffer from a well-acknowledged problem of long-term wear resulting in osteolysis, implant loosening, and revision surgery. With revision surgery being a costly and painful procedure, there is a need for longer-lasting knee replacement technology. Additionally, with the limited lifetime of current artificial knee joints, there is an unaddressed portion of individuals suffering from osteoarthritis who are not candidates for total knee replacement. Rogue Orthopedics has developed the SpringSert, a medical device that will be capable of incorporation into a standard artificial knee joint and provide a passive unloading mechanism to reduce stress in the implant and extend its lifetime. Our technology will allows individuals suffering from knee osteoarthritis to receive earlier joint replacement and thus, obtain early, effective, and lasting pain relief.