2014
Global Health Innovations
-
The Team
Student Team: Kevin Keenahan, Pratik Patel, Anant Subramaniam, Tiffany Tseng, Brock Webberman
Medtronic Team: Yong Cho, PhD, Wade Demmer, Subham Ghosh, PhD, Vanessa Pau
Clinical Advisors: Aravindan Kolandaivelu, MD, Department of Cardiology; Harikrishna Tandri, MD, Department of Cardiology; Calambur Narasimhan, MD, DM, Care Hospital, Hyderabad, India; Soumyadipta Acharya, MD, PhD, Department of Biomedical Engineering
Advisors: Dr. Vinod Sharma, PhD, Medtronic, Inc.; Naresh Pagidimarry, Glysure ?????
Abstract
Cardiac arrhythmia patients in the developing world can often go many years of experiencing symptoms such as dizziness and fainting, among others, without receiving proper care. Based on epidemiological data around 1.3 million cardiac arrhythmia patients should receive a pacemaker every year. Yet in 2009 only 20 thousand patients had access to this treatment and not much has changed since then. This team at Johns Hopkins is collaborating with Medtronic to identify and address the key bottlenecks for the appropriate diagnosis and treatment of cardiac arrhythmias in targeted Indian demographics. Early on the underserved segment was identified as a critically important population. These individuals have neither the access nor the capabilities to seek care for their arrhythmia ailments. Incorporating this population would not only lead to the downstream increase in pacemaker implantations but would also increase access to lifesaving interventions for millions of patients in dire need.
From ethnographic research in the field the team found the largest clinical opportunity was at the beginning of the care pathway with the Rural Healthcare Practitioners (RHCPs) who serve as the first line of care for roughly 65 percent of the Indian population. To ameliorate this systems-level problem, the team is developing a low-cost tablet device that improves the diagnostic capabilities of RHCPs for a variety of common medical conditions, including cardiac arrhythmias. The tablet leverages established clinical decision support system (CDSS) algorithms, but caters specifically to the disease states seen commonly by RHCPs to help them decide whether to keep a patient for treatment or refer them to a specialized doctor, such as a cardiologist. The system also includes an electrocardiogram (ECG) plug-in that allows RCHPs to perform ECGs within their clinic.
The team has formed a partnership with a local NGO in India, JSV Innovations, to implement field studies. A preliminary ECG monitor and CDSS system was brought to the field and received positive feedback from our partners in India and RHCPs alike. The team will be implementing a more developed prototype to further iterate on this concept and better understand the impact on a workflow and financial standpoint. By developing a system to empower the diagnostic abilities of lower levels of the healthcare system, we believe we can ultimately improve the diagnosis and treatment of cardiac arrhythmias in developing countries.
-
The Team
Student Team: Eric Ashuckian, Jennifer Gilbertson, Julia Michalow, Matthew Petney
Clinical Advisors: Azadeh Farzin, MD, Department of Neonatology; Wilson Wang, MD, Jhpiego Indonesia; Elizabeth Cristofalo, MD, Department of Neonatology
Advisors: Kristy Peterson, Product Develop Manager, Jhpiego; Lindsay Litwin, Senior Program Coordinator, Jhpiego; Luke Mullany, PhD, Department of International Health, Bloomberg School of Public Health; Joanne Katz, ScD, MS, Department of International Health, Bloomberg School of Public Health; Pushkar Ingale, Laerdal Global Health, India; Jinjie Sunny Chen, Laerdal Global Health, Norway; Tor Inge Garvik, Laerdal Global Health, Norway
Abstract
Neonatal hypothermia affects an estimated 17 million newborns annually in developing countries. It is a significant contributing factor to the high rates of neonatal mortality that exists in this setting because hypothermia compromises neonates’ immune systems, thus increasing their susceptibility to other conditions such as infection and hypoglycemia. In Nepal neonatal hypothermia is the fourth leading cause of neonatal death and 16 percent of hypothermic neonates die during the first week after birth.
Despite high incidence rates for hypothermia, caretakers are frequently unaware of its occurrence because the early stages of hypothermia are asymptomatic. Our team has developed the IllumiNate hat to monitor neonatal temperature and alert care providers when newborns become hypothermic. The hat uses a low cost circuit that lasts for a minimum of three days, the highest risk period for hypothermia and its associated mortality. The alert is designed to be easily interpreted by non-literate mothers. Field studies in Nepal, Tanzania, and India have confirmed the need for hypothermia prevention and monitoring, and have guided the team’s design process. Bench-top testing has additionally demonstrated that the technology is comparable to the standard of care. The IllumiNate hat will be implemented with a training program on hypothermia prevention and management, and will empower mothers to monitor their babies for hypothermia, one of the most risky and easily corrected conditions that newborns face.
-
The Team
Student Team: Melissa Diskin, Jan Lee, Pankti Shah, Barrett Yates
Clinical Advisor: Cherrie Evans, DrPH, CNM, Jhpiego
Advisors: Helge Fossan, Laerdal Global Health, Norway; Jinjie Sunny Chen, Laerdal Global Health; Harshad Sanghvi, MD, Jhpiego; Lynn Kanyuuru, MD, Jhpiego; Kristy Peterson, Jhpiego
Abstract
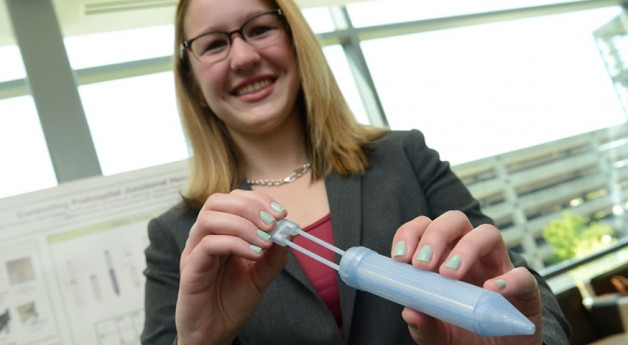
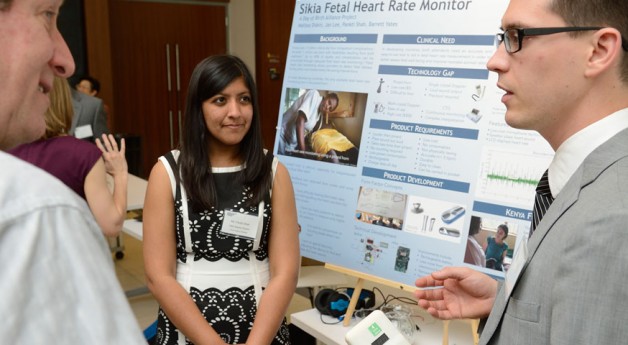
Each year, two million babies die annually from intrapartum-related deaths. Another one million are born with defects caused by birth asphyxia. To prevent complications the World Health Organization recommends that providers measure and record fetal heart rate every 30 minutes. The fetal heart rate provides critical information that determines if an intervention needs to be performed. Studies have shown that up to 43 percent of intrapartum neonatal deaths could be related to inadequate fetal heart rate monitoring. The current monitoring device, the Pinard horn, is inaccurate, time-consuming, fatiguing and difficult to use. When providers are unable to effectively monitor fetal heart rate during labor, it compromises the providers’ abilities to take action.
In partnership with Jhpiego and Laerdal Global Health, the design team has developed the Sikia monitor, an electronic fetal heart rate monitor that plays the fetal heart sound and displays heart rate. By using simple, inexpensive microphone technology, providers will have a faster, easier, and more accurate way to measure fetal heart rate. The team has recorded fetal heart sounds, improved signal quality, and has started developing an algorithm to calculate heart rate. The team has also received feedback by conducting interviews with midwives through Jhpiego, and through field visits to hospitals in India, Nepal, and Kenya. Additionally, the team has designed a study at a high-volume facility in Thika, Kenya to be performed this May. This study will provide additional users validation and feedback and quantify the value of the Sikia monitor over other devices. Overall, the Sikia monitor will increase the frequency of fetal heart rate measurement during labor, allowing for more timely interventions and thereby reducing the incidence of stillbirths and neonatal morbidity.
-
The Team
Student team: Joshua Budman, Kevin Colbert, Aaron Enten, Michael Parlato, Ashley Polhemus
Advisors: Harshad Sanghvi, MD, Jhpiego; Soumyadipta Acharya, MD, PhD
Abstract
Anemia in Developing Countries
Anemia during pregnancy is defined as hemoglobin (Hb) concentration less than 10g/dL. Maternal anemia affects more than half of the pregnant women worldwide, causing 100,000 maternal deaths and 600,000 neonatal deaths each year. It also leads to poor outcomes for the child in the form of preterm birth, low birth weight, malnutrition, and stunted cognitive development. If it is identified early, cost effective therapies can combat the effects of anemia on the mother and the child. In fact, ferrous sulfate tablets have been shown to cure anemia if the patient is adherent. However, low adherence (<50 percent in many Asian and African countries) has been reported among pregnant women. In these populations, anemia is rarely caught early in pregnancy. If women are screened regularly, they can be informed of their anemic status and may be more likely to adhere to their recommended iron supplementation regimen. HemoGlobe: A Point of Care Hemoglobin Assessment Tool
HemoGlobe is a new paradigm in preventative medicine that will empower community health workers to take anemia screening to the doorstep of rural women. A low-cost, noninvasive sensor passes multiple monochromatic lights through the finger and onto a photo detector. Using principles of photoplethysmography, the device collects the transmitted light and processes the resulting waveform. The device then connects to a cell phone, allowing real time analysis of the waveform and classification of the patient as having severe, moderate, or mild anemia. Preliminary results are based on waveforms that were collected from approximately 500 patients in Nepal and eastern India. These waveforms were subjected to a variety of nonlinear regression techniques, neural networks, and a support vector machine to develop the calibration curve.After the waveform is collected patient data can be documented on the cell phone and, along with their anemia assessment, sent to a central server via SMS, MMS, phone call, or email. Uploading this data either to a server or the cloud creates a real-time database of anemia prevalence and distribution. This database can be used to track progress in areas with a disproportionate burden of maternal anemia, as well as facilitate resource allocation decisions by public health organizations. Use of this device on an international scale has the potential to reduce rates of maternal mortality, prevent premature births, and increase the health of young children in developing countries by facilitating point of care medical assessment and education for mothers with limited access to healthcare.
U.S. Healthcare Innovations
-
The Team
Student team: Aaron Enten, Julia Michalow, Ashley Polhemus, Brock Webberman
Clinical Advisors: Michael Boland, MD, PhD, Department of Ophthalmology; William Anderson, MD, PhD, Department of Neurosurgery; Deborah Stein, MD, MPH, Shock Trauma Center at University of Maryland Medical Center; Wendy Ziai, MD, Department of Neurology; Betsy Zink, MS, RN, CCNS, CCRN, CNRN, Neuroscience Critical Care Unit
Abstract
Headaches in the Emergency Department
Each year, six million patients visit emergency departments (ED) in the United States (US) with headache as their primary complaint. While many of these patients are seeking treatment for intolerable, recurrent headaches such as migraines, up to 15percent of patients suffer from serious neurological conditions with emergent underlying pathologies. These high risk conditions are not easily discernable from benign headaches and can be fatal, requiring urgent diagnosis and treatment. However, neurological crises are misdiagnosed as migraines in up to 25percent of cases, resulting in wrongful discharge from the hospital, worse outcomes, and a higher chance of mortality.
Elevated intracranial pressure (ICP) is not only a symptom of many of these conditions, but also an independent point of concern, and treatment to reduce ICP is vital for preventing permanent brain damage. Some of the first observable symptoms of raised ICP occur in the eye. However, high intra and inter-observer variability during ophthalmic examinations have been reported of physicians in the emergency room and this prevents these tests from being used at the point of care.
InSpect: A Physician’s Aid for Timely Diagnosis
The inSpect system takes the skill of the ophthalmologist and places it in the hands of the emergency care provider. The inSpect digital ophthalmoscope collects video of the eye and uses processing software to automatically measure several key ophthalmic parameters on the pupil and the back of the eye. These parameters include abnormal pupillary response to light, papilledema, venous engorgement, and spontaneous venous pulsations. Our software leverages masking techniques used to detect and isolate the vasculature, with blob detection algorithms used to measure and track both the pupil and the optic disk. Videos are stabilized mechanically with a disposable eyepiece, as well as using digital rendering and point feature mapping. Our current eyepiece prototypes have been shown to reduce video instability due to hand movements during examinations by up to 90 percent.
Videos are analyzed to provide a real-time assessment of intracranial pressure, which is indicative of neurological crisis. Care providers can thus integrate this ophthalmic assessment with the physical examination for more accurate and timely differentiation between high and low risk headaches. Patients will benefit from faster administration of therapy and more reliable therapeutic decision-making to achieve optimal outcomes.
-
The Team
Student team: Matthew Petney, Eric Ashuckian, Jan Lee, Pankti Shah, Tiffany Tseng
Clinical Advisors: Roy Brower, MD, Department of Pulmonary and Critical Care Medicine; Brendan Canning, PhD, Department of Allergy and Clinical Immunology; Geetika Sood, MD, Department of Infectious Diseases; Julianne Perretta, MSEd, RRT-NPS, CHSE, Johns Hopkins Simulation Center; Katie Mattare, RT, Department of Adult Respiratory Care
Abstract
Annually, approximately 800,000 patients rely on mechanical ventilation (MV) delivered through a breathing tube to survive. Over time the presence of a breathing tube prevents the elimination of bacteria that build up in the lungs. Within a matter of days patients on ventilation often develop complications and secondary infections that worsen their condition. For instance, ventilator-associated pneumonia (VAP) increases a patient’s hospital stay by two weeks and is directly responsible for 36,000 deaths each year. Based on historic Medicare data, only 83 percent of ICU costs are compensated. ICU cases with complications and infections significantly lengthen a patient’s stay, causing the hospital to lose money. Each day in the ICU costs the hospital $3,200. When a patient develops a secondary infection such as VAP hospitals are not reimbursed for the additional resources used and lose on average $12,000 per patient.
Coughing is one of the body’s main defenses against respiratory infection. The breathing tube prevents ventilated patients from coughing effectively because it prevents the closure of the glottis, which in turn does not allow sufficient pressure to build up in the lungs. Our device, the PreVent, is a ventilator attachment that restores a patient’s ability to effectively cough and integrates seamlessly into the intensive care unit (ICU) workflow.
Preliminary data has shown that briefly obstructing the airway during an exhalation, as the PreVent does, creates an effective cough profile. The team has also performed safety testing at the Johns Hopkins Simulation Center to ensure that the PreVent does not interfere with a patient’s ventilation therapy. Over the next few months the team will perform bench testing to demonstrate efficacy in moving mucus. In addition, an IRB study has been submitted to gather flow and pressure characteristics directly from mechanically ventilated patients to develop the cough detection system.
The PreVent will help hospitals save thousands of dollars in patient care and excel in quality metrics. Most importantly, by allowing patients to safely eliminate mucus from their lungs the PreVent will improve the respiratory function of critical care patients, prevent secondary infections, and expedite recovery.
-
The Team
Student team: Kevin Colbert, Jennifer Gilbertson, Michael Parlato, Pratik Patel, Barrett Yates
Clinical Advisors: Ashish Nimgaonkar, MD, MS, MSc, Department of Gastroenterology; Pankaj Pasricha, MD, Department of Gastroenterology, Bayview Medical Center; Thomas Donner, MD, Department of Endocrinology; Lawrence Cheskin, MD, Weight Management Center, Bloomberg School of Public Health; Hien Nguyen, MD, Department of Surgery, Bayview Medical Center
Abstract
Type 2 Diabetes: A Shift in Thinking?
Twenty five million Americans live with type 2 diabetes mellitus (T2DM) in the United States. Traditionally, T2DM has been treated with insulin therapy and oral hypoglycemics which compound over a patient’s lifetime, cause weight gain, and lead to greater insulin resistance. Bariatric surgery has been shown as an extremely promising treatment for T2DM as recognized by the American Diabetic Association. However, very few patients qualify for surgical treatment and are willing to accept the risks inherent to the invasive procedure. Research over the past several decades has pointed to exclusion of the proximal gut from contact with nutrient flow as the cause of diabetic remission.
The Stasys Approach
After conducting an extensive literature search and speaking with leading bariatric surgeons, endocrinologists, and gastroenterologists, the Stasys team has identified a novel device-based approach to mimic the metabolic effects of surgery while minimizing risks. Exclusion of the intestine from alimentary flow is achieved via an intestinal lining delivered by orally ingested capsules. The mechanism of our first-generation devices has been validated using a bench-top peristalsis model. Furthermore, several proof of concept in-vivo rat studies have validated the impact of our approach on blood glucose levels. Stasys is on track for large animal experiments to validate the safety and efficacy of our device. Patients, providers, and payers have expressed support of the Stasys treatment due to the early demonstration of efficacy, low risk profile, and cost of the device. The Stasys approach has the potential to improve the lives of millions of type 2 diabetics in the United States and beyond.
-
The Team
Student team: Joshua Budman, Melissa Diskin, Kevin Keenahan, Anant Subramaniam
Clinical Advisors: Leigh Ann Price, MD, Department of Plastics and Reconstructive Surgery; Susan Rhee, MD, Wound Healing Center, Bayview Medical Center; Gabriel Brat, MD, MPH, Department of Surgery; Alex Kor, DPM, Department of Orthopaedic Surgery; Lew Schon, MD, Department of Orthopedic Surgery, Union Memorial Hospital
Abstract
Wound care is not glamorous but a $20 billion global market is hard to ignore. Most of us could not imagine living with an open sore, but 8 million Americans do. Chronic wounds, defined as those that do not heal for more than six weeks, are on the rise due to the increase in patients with comorbidities such as diabetes, obesity and old age. These wounds are often composed of dead and infected tissue which must be removed in order for the wound to heal. Debridement, or removal of the dead tissue, is performed by a specially trained clinician who cuts out the dead tissue with a scalpel. Wound healing progress is measured through both area reduction and change in tissue composition from dead and infected tissue to ingrowth of new healthy tissue. Wound area measurement and tissue composition, both crucial metrics to determining the success of wound treatment, are currently performed visually, implying a highly subjective process that can have errors of up to 40 percent. Patients require debridement procedures at a high frequency, making chronic wound care an expensive and labor-intensive process. With the cost of treatment continuing to skyrocket the wound care market needs a solution which will reduce costs by increasing healing rates and deskilling wound care, allowing more patients to continue treatments at home instead of in a specialized care setting.
Tissue Analytics proposes to change the way wound care is conducted. The WoundMEND System consists of three proprietary components: WoundSTIM, a microneedle injection with an FDA-approved enzymatic debriding agent; WoundCAP, a bristle-coated dressing for continuous debridement; and WoundTRACK, an app that tracks wound healing. The system is designed to be used at home and can be implemented by a home-care nurse instead of a clinician. With a simple photo taken by the user wound healing can now be monitored at home on the WoundTRACK App, which can measure many parameters that cannot be determined with visual inspection. To dress the wound WoundSTIM is used to deliver the enzymatic debriding agent within large areas of necrotic tissue, breaking it down faster than the standard of care. Rat studies in over 60 necrotic wounds show that WoundSTIM application causes a 20 percent increase in blood flow to the wound, an important indicator of healing. The WoundCAP dressing acts as a real-time and continuous care provider removing necrosis and biofilm as it develops.
Tissue Analytics is pursuing a staged developmental strategy focusing initially on building and commercializing the WoundTRACK App. On building credibility and ensuring a consistent revenue stream we will introduce both the WoundSTIM and WoundCAP technologies to move wound monitoring and healing to the patient’s home. In this way, the WoundMEND System can autonomously care for wounds with a substantial increase in frequency of wound monitoring and unprecedented instantaneous intervention. Use of the WoundMEND System is projected to increase healing rates by 25 percent and save payers 50 percent over the cost of care for a single wound.